David Pigott, MD, RDMS, FACEP
Bobby Lewis, MD, DDS, FACEP
Chris Johnson, MD
40M reports near-total vision loss and eye pain after being struck in left eye during an altercation. He states he has ~95% vision loss in the affected eye and can only see in the superior portion of his visual field. He states his eye pain is mild and is not worsened with ocular movement.
The patient reports a history of opiate abuse on suboxone.
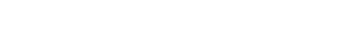
Point-of-care ultrasound (POCUS) was performed:
Note the appearance of well-defined, serpentine linear structure within the posterior chamber consistent with retinal detachment (RD). This structure does not appear to be tethered to the optic disk, suggesting “mac-off” retinal detachment, where the retina has been separated from the macula. In “mac-on” retinal detachment, central vision is preserved, although emergent retinal repair is still indicated to prevent progression to “mac-off” RD.
A recent case report with excellent discussion on RD is here: https://jetem.org/retinal_detachment/
The patient was evaluated by ophthalmology and the diagnosis of retinal detachment was confirmed. The patient was taken for operative repair at Callahan Eye Foundation Hospital.
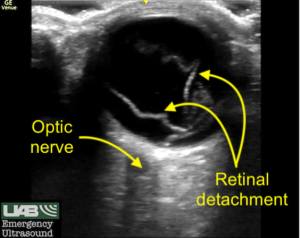
Large or complete retinal detachments may have a characteristic V shape, where the point of the V indicates the insertion into the optic disc/optic nerve (ON). This is an example of “mac-on” RD.

A recent review of the use of POCUS for the detection of retinal detachment in the ED setting can be found here:
Lahham S, Ali Q, Palileo BM, Lee C, Fox JC. Role Of Point Of Care Ultrasound In The Diagnosis Of Retinal Detachment In The Emergency Department. Open Access Emerg Med. 2019 Nov 13;11:265-270.
Another common finding on ocular POCUS is vitreous hemorrhage. Patients may present with a range of ocular complaints, including the presence of “floaters” or even total visual loss. Absence of the “red reflex” may also suggest the diagnosis of vitreous hemorrhage.
On ultrasound, the characteristic “washing machine” sign, caused by the to-and-fro movement of echogenic blood within the posterior chamber, can be seen. [image not provided given this document can only include still images and to see the washing machine sign a video image is required].
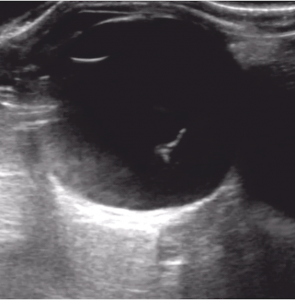
Distinguishing between retinal detachment (RD) and posterior vitreous detachment (PVD), another common ocular disorder, can be difficult. Retinal detachment typically presents as a hyperechoic line that does not cross the optic nerve, is uniformly thick, more echogenic when compared to a PVD, and less mobile with ocular movements. PVD may present as a hyperechoic line that can cross the optic nerve, has varying degrees of thickness, is less echogenic when compared to a RD, and is more mobile with ocular movements.
Lahham S, Shniter I, Thompson M, Le D, Chadha T, Mailhot T, Kang TL, Chiem A, Tseeng S, Fox JC. Point-of-Care Ultrasonography in the Diagnosis of Retinal Detachment, Vitreous Hemorrhage, and Vitreous Detachment in the Emergency Department. JAMA Netw Open. 2019 Apr 5;2(4):e192162.
An example of a vitreous detachment is seen here. Note the present of a thin mobile echogenic membrane that clearly crosses the optic disc/optic nerve.
A good discussion of retinal vs. vitreous detachment is available from the emergency ultrasound folks at Emory.
It is important to optimize the gain during ocular studies, as low gain may obscure important findings in the posterior chamber. Also, remember to use the Ocular or Ophthalmic presets when performing ocular ultrasound. The FDA restricts the amount of ultrasound energy that should be used during ocular ultrasound due to concerns over potential retinal injury caused by excess mechanical energy propagated by ultrasound waves.
As always, the ALARA (As Low As Reasonably Achievable) principle should be followed during all POCUS exams, indicating that ultrasound operators should limit patient ultrasound exposure while maintaining diagnostic quality.
Additional discussion of ultrasound bioeffects can be found here:
Nelson TR, Fowlkes JB, Abramowicz JS, Church CC. Ultrasound biosafety considerations for the practicing sonographer and sonologist. J Ultrasound Med. 2009 Feb;28(2):139-50.